

Seeking a way to break the cycle of addiction for yourself or a loved one is the first major step toward sobriety - learn where to begin.
Underestimating the need for addiction treatment is common - most do it. Interventions offer a way to recommend help for a loved one who refuses treatment.
A vital step towards physical healing, detoxification is the process of weaning the body free from addictive substances in a safe, medical atmosphere.
Individual and group therapy sessions are a key component to recovery. Here patients will learn how to safely cope with past trauma and current triggers that could lead to relapse.
Immediately following a drug or alcohol detox regimen, patients spend time in a residential or inpatient rehab program that focuses on restoring both physical and mental health.
During treatment, each patient develops effective coping mechanisms to help them face everyday challenges without the use of drugs or alcohol.

Over 140 people in the United States are dying each day from an opioid overdose. Opioids are a class of drugs that include illegal substances such as heroin, and fentanyl, and prescription medication such as oxycodone. Both illicit and legal opioids can cause addiction, and overdose.
The CDC estimates that six people die every day from alcohol poisoning with over 88,000 Americans dying annually from an alcohol-related illness. Alcohol use disorders are the third leading cause of preventable death in the United States. Early intervention and proper treatment can help stop alcohol from taking another life.
Meth, also known as methamphetamine or crystal meth, is a highly addictive substance that impacts your central nervous system. Meth abuse can cause severe mental and physical side effects, including changes to the brain. Stop long-term damage by seeking out treatment now.
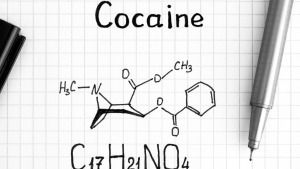
NIDA estimates over 35 million Americans abuse cocaine, and 8.6 million abuse crack cocaine. Cocaine is an extremely addictive substance that causes over 400,000 emergency room visits each year, many of which are to treat an overdose.
 How is Crack Cocaine Addiction Treated?
How is Crack Cocaine Addiction Treated?
Highly addictive and extremely popular, crack cocaine is a widely abused drug in the United States. Due to its prevalence, the need for crack-specific drug rehab programs has developed. Crack is a form of cocaine, making it a central nervous system stimulant. It is made by combining cocaine with water and baking soda or ammonia …
Read More Recovery From a Transgender Perspective
Recovery From a Transgender Perspective
It’s not surprising that the transgender community disproportionately experiences anxiety, depression, and even chemical dependency. Trans individuals report feelings of confusion and low self-esteem, while also dealing with discrimination, misunderstanding, harassment, and exclusion. In order to combat the addiction epidemic and highlight Pride Month, we shine a light on recovery in the transgender community. The …
Read More Federal Agencies Finally Go After Internet Drug Dealers
Federal Agencies Finally Go After Internet Drug Dealers
Internet drug dealers are peddling poison online. Deadly pills are being sold through the dark web. And people across the nation are dying from overdoses. Drug markets on the dark web emerged around 10 years ago. Since then, these illegal sales have grown into a multi-million-dollar industry. The United Nations Office on Drugs and Crime …
Read More I’m Going to Rehab – What Should I Tell My Employer?
I’m Going to Rehab – What Should I Tell My Employer?
Taking time out of your life – and time off work – to go to rehab is a huge step. While addiction treatment may feel like a daunting prospect, it will definitely improve your life for the better. You may also be feeling anxious about what to tell your employer. Maybe that fear is something …
Read More